Our bodies play host to many different micro-organisms such as bacteria, viruses, fungi, and foreign cells. The study of microbes has exploded with the recent advances in microelectromechanical systems (MEMS) and specifically microelectronics. But aren’t microbes bad?
They’re technically foreign objects and outnumber our cells, but most are completely harmless, and some are, in fact, critical to normal bodily functions. Our microbiome changes on a daily basis as we vary things like diet, drug intake, stress, and other environmental factors, but let’s start at the beginning of microbiome analysis and how electronics have “stimulated” physiological research and excelled our understanding of the human anatomy.
A brief history of implantable electronics
Implantable electronics have been around for over six decades, with the first application dating back to just a few years after the transistor was invented and frequency-modulated (FM) radio signals were established. In 1959, Mackay Noller and others developed and tested radio transmitters that communicated physiological information from within the human body, primarily the gastrointestinal tract. Shortly after that, other researchers incorporated biotelemetry units to measure and report information on the human biome in a variety of body cavities without disturbing physiological parameters and optimizing sensing techniques and data transmission. The first major generation of implantable (and swallow-able) biotelemetry in the 1960s reported cardiovascular (electrocardiogram [ECG], blood pressure, and flow), respiratory (oxygen and temperature), neurophysiological (nerve activity), and gastrointestinal (pressure, pH, and temperature) parameters. Figure 1 shows a couple of telemetry circuits from the 1960s.
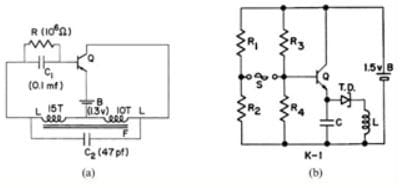
Figure 1: Examples of implantable telemetry systems from the 1960s: a) Mackay-Blocking Oscillator and b) Ko-Tunnel Diode Telemetry Unit (Image courtesy of article “Early History and Challenges of Implantable Electronics", by Wen H. Ko)
By the late 1970s, biotelemetry technology had progressed at rocket speed with more advanced and long-term applications ranging from pacemakers, nerve stimulators, insulin dispensers, and even sports medicine applications such as intra-cranial pressure (ICP) monitoring. Figure 2 shows a battery-less system that radiates a frequency proportional to surrounding cranial pressure used for head-trauma analysis.

Figure 2: Intra-cranial pressure telemetry system used for head-trauma analysis (Image courtesy of white paper “The Advantages of Short Range Telemetry though intact skin for Physiological Measurements in both Animals and Man", by T. B. Fryer)
Today’s world of human microbiome analysis features highly sophisticated electronic devices and technology, so let’s explore some of the more recent developments and applications.
MEMS technology and its applications in the microbiome
Organ-on-a-chip is a relatively new technology utilizing a combination of microfluidics, biomedical microelectromechanical systems (or bioMEMS), and biomaterial to mimic and simulate multi-level organ systems on a lab bench. This allows for real in-vitro studies such as drug testing or disease research while also developing useful implantable function-assistant devices. Brain, liver, heart, kidney, lung, and intestine functions have all been successfully implemented on a chip platform and have integrated various types of electronics.
Many organ-on-a-chip devices incorporate microsensors (or MEMS sensors) that assist with transducing things like pH, temperature, pressure/force, acceleration, humidity, sound/vibration, magnetic fields, and other biological or chemical parameters into an electrical signal. These microsensors almost always include a mechanical element (such as a diaphragm or cantilever beam) integrated with other microelectronics in a very small form factor but generally require some sort of signal processing and calibration or compensation to interface with it. Capacitive sensors are one of the most common sensing techniques used in MEMS devices and generally have a very small range. There are many ways to convert a variable capacitance to a measurable signal such as an oscillator or bridge. See Figure 3 for some examples of these analog interfaces.

Figure 3: Methods for the measurement of capacitance changes: (A) bridge, (B) and (C) current-voltage measurement — single/differential, (D) frequency measurement, and (E) time measurement (Image courtesy of book “Sensors for Mechatronics" (Second Edition), by Paul Regtien and Edwin Dertien)
Many digital MEMS sensors have these interfaces integrated inside the device and provide an easier interface such as a TTL-level analog output or serial bus such as I2C or SPI. Whether used in an implantable device, organ-on-a-chip, or in other non-medical industries, MEMS technology and research continues to flourish as we improve our ability to manufacture and micro-machine electromechanics on a microscopic scale. Many MEMS devices such as flow, temperature, humidity, and motion sensors can be found on Arrow Electronics.
Challenges associated with implanting electronics and designing bio-electromechanics
There are many difficulties associated with implanting or interfacing an electronics device with a human body, including minimizing size, weight, and power consumption while protecting the circuitry from the harsh and humid environment. And above all, the device must be safe and reliable.
Let’s start with size. How do you make something as small as possible without sacrificing performance? It helps to have a design process that allows mechanical and electrical engineers to work very closely together on optimizing package and mechanical layout, and CAD systems today have progressed by leaps and bounds over historical design methodologies in allowing complete visualization before any hardware is even produced.
But reliability is a big one, too. Many implanted and bioMEMS electronics are hermetically sealed by a process called “potting,” which creates a hardened, gelatinous barrier between the components and the enclosure. And depending on the classification rating of the medical device (implantables are generally Class III, the highest risk class), certain IEC standards will require it to be tested against rigorous safety protocols and require backup functions and redundancies.
And lastly, power optimization (particularly for implantables) has been a constant battle for engineers. We’d like to think we can tap into Iron Man’s Arc Reactor core power source, but instead, we use small batteries, supercapacitors, energy-harvesting techniques, and highly optimized low-power features of components. In-vivo energy harvesting (IVEH) has been a recent area of exploration that utilizes piezoelectric and triboelectric effects, endocochlear potential, biofuel cells, and light to provide ways of trickle charging batteries or capacitors. In 2014, a research team from Korea developed a pacemaker that is powered completely by flexible piezoelectric material, called a “nanogenerator.” See Figure 4 for an illustration of the pacemaker’s power path.

Figure 4: Artificial cardiac pacemaker using electrical energy from a flexible piezoelectric material (Image courtesy of white paper “Self-powered cardiac pacemaker enabled by flexible single crystalline PMN-PT piezoelectric energy harvester", by Geon-Tae Hwang and team at KAIST)
Examples of implantables, microbiome-on-a-chip, and bioMEMS products
We’ve discussed the evolution of microsensors/microelectronics and how they’ve been used in the human microbiome and simulated organs, but now let’s see them in action.
French company Biomillenia, in combination with QIAGEN’s microbial bioinformatics platform, has developed a droplet-based microfluidics chip platform used for culturing and analyzing microbes and bacterial species at an unparalleled level. Their platform can screen up to 100 million microbes in three days, whereas traditional methods would take up to three years while requiring a much larger volume for analysis.
At Tufts University, Fiorenzo Omenetto has studied how to use silk with an LED array as a dissolvable, implantable device to indicate the concentration in the blood of biomarkers, like insulin. The idea is for the silk to hold the LED/transistor array in place, then use antibodies or enzymes to detect biomarkers or disease markers, and then eventually dissolve and leave behind the silicon electronics without the need of surgery for removal.
The CardioMEMS HF System (seen in Figure 5) by Abbott is an implantable device utilizing MEMS technology that proactively monitors blood pressure and wirelessly transmits to a base unit for patient readout, allowing for reduced heart failures and indications before the symptoms even appear. It also opens up options for telemedicine and personalization of patient treatment plans based on the measurements produced by the device.

Figure 5: CardioMEMS device by Abbott that proactively monitors and transmits blood pressure data (Image: Abbott)
Biolinq has implemented a micro-array device (seen in Figure 6) that assesses your glucose levels and trends and will tell you how diet and exercise uniquely impact your blood glucose on a patch the size of a nickel. The patch contains a sensor array, battery, and a circuit board that wirelessly transmits info to an app.
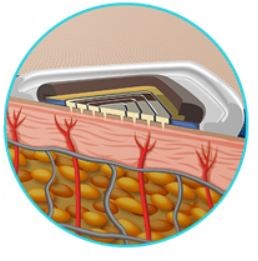
Figure 6: Biolinq’s micro-array device that monitors blood glucose (Image: Biolinq)
Innovative Sensor Technology (iST) has developed biosensors used to measure concentrations of glucose, lactate, glutamine, and glutamate by using various electrodes that sense current as low as 20 pA. That’s 20-million-millionths of an amp!
And Sensera, a company that specializes in IoT sensor solutions and microfabrication, has developed commercially viable lab-on-a-chip and organ-on-a-chip diagnostics utilizing its patented microsensing and microfluidics technologies. Figure 7 shows an example of microsensors used in an organ-on-a-chip application. Many Sensera MEMS and IoT products are available at Arrow Electronics.
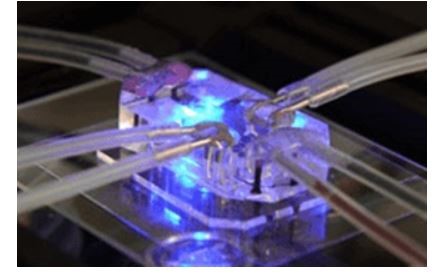
Figure 7: Sensera’s microsensors used in an organ-on-chip application (Image: Sensera)
What will medical science look like a decade from now? We’re living in the age of science fiction becoming a reality, and it’s exciting to think of how bioMEMS and microbiome-on-a-chip applications will continue to unfold and push the boundaries of how we can measure and analyze parts of the human anatomy.


